Introduction: During red blood cell (RBC) transfusion, exposure to unmatched non-ABO antigens can lead to production of alloantibodies that promote potentially fatal hemolytic events. Patients with Sickle Cell Disease (SCD) have the highest incidence of RBC alloimmunization. Prior studies indicate that an altered immuno-regulatory and/or pro-inflammatory state may determine the risk of RBC alloimmunization. For example, one study reported that patients with SCD have inflammatory cytokine gene polymorphisms that could be associated with diverse disease presentations and alloimmunization. We previously reported that inflammatory type 1 interferons (IFNα/β) produced by innate immune cells are required for RBC alloimmunization in mice, while others have suggested that NFkB-induced cytokines play a role in murine transfusion models. However, the inflammatory factors that regulate RBC alloimmunization in patients with SCD are poorly understood. Alloimmunized patients with SCD also have elevated levels of anti-RBC autoantibodies, which facilitate erythrophagocytosis. Given the role of erythrophagocytosis by spleen macrophages in processing RBC antigens, we hypothesized that erythrophagocytosis of SCD RBCs may promote inflammatory pathways that regulate alloimmune responses.
Methods: RBCs from control subjects (AA), and reticulocytes and mature RBCs from patients with SCD, were opsonized or not with anti-RBC antibodies (anti-RhD) and co-cultured for 3 hrs with human macrophages (hMac) differentiated from monocytes of healthy subjects. Phagocytosis of labeled RBCs was analyzed by flow cytometry. Bulk mRNA sequencing of co-cultured macrophages was performed to identify differential gene expression. Ingenuity Pathway Analysis (IPA) software was used to identify relevant pathways and upstream regulators of differentially expressed genes. To validate sequencing results, cytokine levels from co-culture supernatants were measured by multiplex cytokine assays.
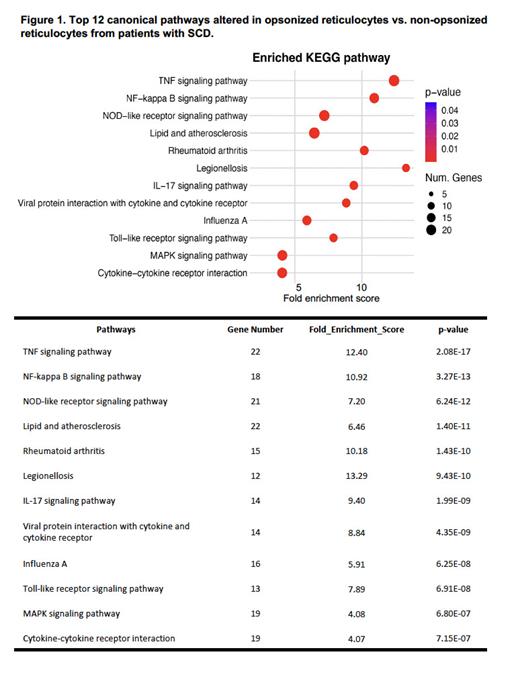
Results: Flow cytometric analysis revealed that opsonization was required for erythrophagocytosis in an FcR dependent manner. RNA-seq Differential Expression analysis of macrophages co-cultured with AA opsonized RBCs vs. non-opsonized RBCs identified 166 significantly upregulated and 24 downregulated genes (p<0.0001). IPA analysis revealed that the top 12 canonical pathways were related to inflammation, including TNF, IL-17, NF-kappa-B and NOD-like receptor signaling pathways. TNF signaling was the top predicted upstream regulator pathway with a fold enrichment score of 10.3 (16 genes) (p<0.0001). Co-cultures of mature RBCs from patients with SCD showed comparable results. When comparing macrophages from co-cultures of opsonized reticulocytes vs. non-opsonized reticulocytes from patients with SCD, 174 genes were upregulated and 31 were downregulated (p<0.0001). Pathway analysis also revealed unique signatures for opsonized reticulocytes from patients with SCD. The top 12 canonical pathways included TNF, NF-kappa-B and NOD-like receptor signaling pathways (Figure 1). The top predicted upstream regulators were TNF and the NF-kappa B signaling pathway with a fold enrichment score of 12.3 (22 genes) (p<0.0001) and 10.9 (18 genes), respectively (Figure 1). Finally, to validate the sequencing results, cytokines levels from supernatants of hMac co-cultures with the RBCs from the patients with SCD and control subjects were measured. Erythrophagocytosis of opsonized reticulocytes and AA RBCs, compared to non-opsonized co-cultures, led to production of NFκB-mediated cytokines, including TNF.
Our results show that erythrophagocytosis of SCD RBCs promote NFκB-mediated TNF production. These results warrant further investigation of the role of NFκB-mediated inflammation in RBC alloimmunization in patients with SCD.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal